Which has a bigger carbon footprint: the airline industry or healthcare? If you guessed healthcare, you’re spot on.
Climate change is one of the biggest challenges of our time, impacting both the planet and our health. Eight years ago, 196 countries signed the Paris Agreement, a major step in global cooperation to fight climate change by reducing emissions and pollution. Since then, the U.S. has introduced its own climate policies, while states and businesses have also made commitments to tackle the issue.
Progress is being made, and on a government level, the Securities and Exchange Commission (SEC) now requires large public companies to report their emissions and how their carbon footprint affects the world. So how can hospitals get involved and why should they?
Healthcare’s Role in Protecting Communities from Climate Change
Healthcare’s climate footprint is significant. It is estimated that 4.6% of global net emissions are from the healthcare sector. Its major drivers come from energy use, landfill waste, water consumption, and air pollution. In a landmark 2019 report, the group Health Care Without Harm calculated that the United States produces the greatest share of the world’s health care emissions and has the highest per-capita health care climate footprint. Aviation, by comparison, is estimated to contribute 2%-5%.
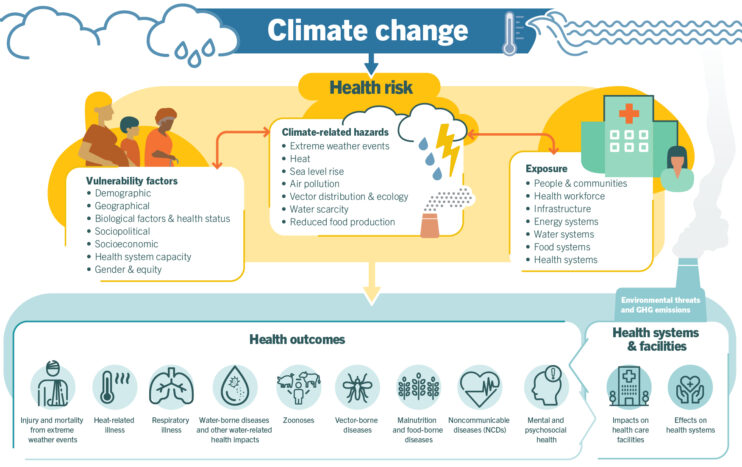
When it comes to our health, the communities we live in have a significant impact on our overall well-being. Pollution and greenhouse gas emissions affect air quality and drive hotter temperatures, exacerbating health issues like asthma, heart disease, heat-related illnesses, and infectious diseases. Vulnerable populations, who already face health disparities, are disproportionately affected by climate change, making it crucial for hospitals to implement climate initiatives that protect these groups and promote health equity.
By investing in climate action, hospitals can reduce emergency department visits, lower patient admissions, and improve both patient and community health through climate action initiatives. These efforts are most impactful when hospital investments are combined with foundation support through blended funding. Foundations can leverage external dollars through grants, donations from individuals or major donors, and partnerships with businesses interested in sustainability and climate action. By working together, hospital foundations and hospitals can magnify the effects of these initiatives, making a greater impact on public health and the environment.
As hospitals conduct their latest rounds of community health needs assessments and implementation planning, the World Health Organization lists these reasons why climate action should be a key consideration:
- Climate change is directly contributing to humanitarian emergencies from heatwaves, wildfires, floods, tropical storms, and hurricanes, and they are increasing in scale, frequency, and intensity.
- Research shows that 3.6 billion people already live in areas highly susceptible to climate change. Between 2030 and 2050, climate change is expected to cause approximately 250,000 additional deaths per year, from undernutrition, malaria, diarrhea, and heat stress alone.”
- The direct damage costs to health (excluding costs in health-determining sectors such as agriculture, water, and sanitation) is estimated to be between $2 to $4 billion per year by 2030.
- Reducing emissions of greenhouse gases through better transport, food and energy use choices can result in large gains for health, particularly through reduced air pollution.
Source: World Health Organization
Climate change disproportionately affects vulnerable populations, particularly those already facing health disparities, but the call for climate action and sustainability is also coming from the workforce. In a recent study by the Deloitte Consumer Center in March 2023 State of the Consumer survey, 69% of employed adults surveyed said the sustainability efforts—such as reducing carbon, using renewable energy, and reducing waste—of their employers are important to them. Employees between the ages of 18 and 34 years old felt stronger about the need for these sustainability efforts compared to older generations.
Hospitals are well-positioned to implement climate initiatives that protect vulnerable groups and promote health equity. Here are a few ways hospitals, foundations, and community partners can work together to improve climate and healthcare outcomes.
Transition to Sustainable Transportation
According to the EPA, greenhouse gas (GHG) emissions from transportation account for about 28 percent of total U.S. greenhouse gas emissions, making it the largest contributor of U.S. GHG emissions. Air pollution is a significant contributor to asthma. Pollutants like ozone, particulate matter (PM), nitrogen dioxide (NO₂), and sulfur dioxide (SO₂) can irritate the airways, triggering asthma attacks and worsening symptoms for those already diagnosed with the condition. Long-term exposure to polluted air can also increase the risk of developing asthma, especially in children and vulnerable populations. Indoor air pollutants, such as mold, dust, and chemicals from cleaning products, can also exacerbate asthma symptoms. In areas with high levels of pollution, asthma rates and hospitalizations tend to be higher, illustrating the direct link between air quality and respiratory health.
As hospitals strive to become more sustainable, they can begin by reducing their carbon footprint through transitioning fleet vehicles to electric or hybrid models. Hospital foundations can play a crucial role by sourcing grants and donations from companies with vested interests in sustainable transportation, and blended funding from both the hospital and the foundation can accelerate the adoption of electric vehicles and other clean transport technologies. Additionally, hospitals can promote the use of electric vehicles (EVs) by installing EV charging stations, making it easier for staff and patients to embrace this eco-friendly option.
In city centers, many hospitals encourage alternative commuting methods and could offer incentives for cycling, walking, or using public transportation, further minimizing the environmental impact of staff and visitors.
How to Measure:
- Percent of hospital fleet vehicles transitioned to electric or hybrid models
- Percent of staff participating in alternative commuting programs
- Percent monthly reduction in GHG emissions from hospital transportation activities
Energy Use to Energy Efficiency
Hospitals operate 24/7, consuming significantly more energy than a typical household. Transitioning from fossil fuels to renewable energy sources like on-site solar panels, wind turbines, or purchasing clean energy from utility providers can lower costs and reduce reliance on fossil fuels.
By collaborating with their foundations, hospitals can access external funding to help finance renewable energy projects. Foundations can apply for sustainability grants or partner with environmental organizations and corporate sponsors that are committed to green energy solutions. This blended approach can ensure that hospitals not only cut energy costs but also enhance the overall impact of their sustainability efforts. By optimizing energy use and implementing sustainable practices, hospitals can realize long-term savings, which can then be reinvested in patient care and community health programs.
Many hospitals are now embracing energy-efficient building designs that incorporate features like natural light, green roofs, and improved insulation. These enhancements not only reduce energy consumption but also improve indoor environmental quality, creating healthier spaces for patients and staff.
How to Measure:
- Percentage of energy sources from renewable sources
- Reduction of energy consumption per square foot of hospital space
- Annual savings from energy efficient initiatives reinvested into patient care or community health programs
Food Waste to Food Reclamation — Adopting Sustainable Food Practices
According to Feeding America, 47 million people in the United States are food insecure. Conversely, goes to waste and is a major waste stream component produced every day by patients, healthcare workers, and visitors. Food waste results when safe and nutritious food is discarded. Food waste generates greenhouse gases in landfills, of which methane has 25 times the global warming potential of carbon dioxide.
Food insecurity greatly impacts health. Research shows that adults who experience food insecurity are 2 to 3 times more likely to have type 2 diabetes.
Hospitals have great opportunities in this area. For example, hospitals should consider creating partnerships with local food banks to donate excess unserved food following food safety regulations. This is another area where hospital foundations can bring in external dollars. Foundations can secure donations or corporate sponsorships to help fund food reclamation programs, expanding their reach and effectiveness.
By leveraging these resources, hospitals can create partnerships that address both food waste and food insecurity, demonstrating a comprehensive community benefit strategy. In addition, hospitals can adopt local food sourcing policies such as buying produce from local farms. Hospitals can also build on-site gardens and farms creating a supply of fresh produce for hospital kitchens and patients. The use of therapeutic gardens is also ideal for patient therapy, which incorporates food as medicine approach to connecting patients with sustainability food practices.
Reducing food waste in hospitals can improve health for food-insecure patients by reallocating excess food to those in need through donation programs. By partnering with local shelters or food banks, hospitals can provide nutritious meals to underserved communities, helping to address hunger and improve overall health outcomes. Additionally, offering more plant-based and sustainably sourced options can support better nutrition for food-insecure patients while reducing the hospital’s environmental impact. These efforts create a healthier community by addressing both food security and environmental sustainability.
How to Measure:
- Percent of excess food donated to local food banks and shelters
- The amount of food waste diverted from landfills through food reclamation initiatives
- Number of meals provided to food insecure initiatives
- Number of on-site gardens and farms created to supply fresh produce
Case Study: The Children’s Hospital of Philadelphia Community Asthma Prevention Program (CAPP)
Asthma is a leading chronic disease in children and often exacerbated by the child’s environment. In fact, the number of people living with asthma increased in 2022 to more than 27 million people. This equals about 1 in 12 people. The city of Philadelphia is home to over 1.5 million people and ranks 35th for ozone pollution nationwide.
Children’s Hospital of Philadelphia (CHOP) has been addressing this challenge since 1997 through its Community Asthma Prevention Program, which works to improve asthma-related outcomes in children. Through CAPP, families can receive in-home education, supplies to reduce asthma triggers in the home, and participate in asthma education classes.
Growing its impact in this field, CHOP launched CAPP+ to address structural issues in homes that contribute to asthma triggers, such as mold, pest residue, and dust, by replacing and repairing roofs, fixing plumbing leaks, removing carpeting, and sealing holes and gaps to keep out pests and water.
Since 2019, CHOP has renovated over 200 homes throughout West and Southwest Philadelphia, where 1 in 4 children have asthma. After the first year of the program, CHOP noticed children had fewer asthma symptoms and exacerbations, and fewer asthma triggers in the home.
“We always recognized the role housing plays in a child’s life but never anticipated taking on a role like this. We are glad we did, since we’re seeing this program is helping children thrive, stay in school, and avoid hospitalizations. It has now become an important part of our commitment to deliver effective, equitable health care,” said Peter Grollman, Senior Vice President of External Affairs at CHOP.
CHOP’s work demonstrates that investing in asthma prevention not only improves public health but also contributes to cleaner air and addresses climate change — offering a model for other cities to follow.
Interested in learning more about improving health equity in your community benefit strategy? Check out the white paper, Equity-Driven Grantmaking: Transforming Hospital Foundations for Community Well-Being.


